The Rise of Digital Health Coaches
Every few weeks, another “AI health coach” appears — promising to interpret your sleep, diet, stress, or glucose and tell you what to do next. To most people, these look like novelties. But they represent something much bigger: the next stage in the long process by which technology keeps pulling more and more activity out of healthcare and into the hands of consumers.
“Stay relaxed and focused. Trust your training and let’s get that glucose down today!”
I’ve written before that the story of modern medicine and modern technology is increasingly a story of shrinking healthcare. Each wave of technology moves one more thing that used to require a professional into the consumer domain — or eliminates the need for it altogether:
Search engines, and now LLMs give patients the ability to self-diagnose, and potentially self-treat, before ever calling a doctor.
Smartphones and wearables turned into continuous health data monitors, logging everything from movement to language use to falls and gait steadiness.
Self-Driving cars aren’t labeled as medical devices, but they’re already reducing the need for trauma care.
Trauma surgeon substitute?
None of these started within healthcare, but each is in a real sense competing with it. This is disruptive innovation in Clayton Christensen’s original sense — and the outcome is a smaller healthcare system, not a bigger one.
The newest turn in this process: digital health coaches.
The interpretation gap
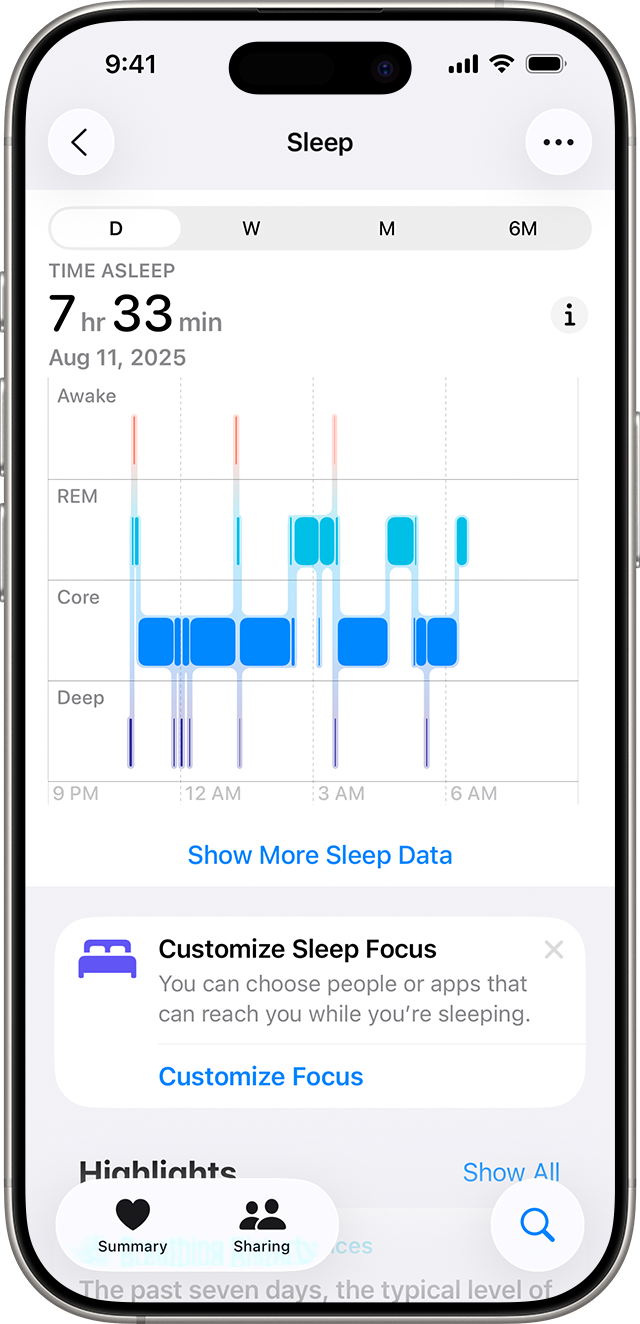
When the iPhone and early wearables appeared, they unleashed an ocean of personal data: steps, sleep, heart rate, oxygen levels, even EKGs. Suddenly, ordinary people were collecting data that previously required a visit to a clinic or lab.
But data isn't understanding. Most people couldn't interpret what their graphs meant or what to do about them. And while healthcare providers have the expertise to make sense of that data, they have no framework or tools to bring it into their systems — and definitely no time to review it during a 10-minute office visit.
So for years, we've had this strange paradox: more health data than ever before, flowing continuously from millions of devices, with almost no one equipped to turn it into action. The data existed. The expertise existed. But they couldn't connect.
That gap — between continuous measurement and continuous guidance — is what AI is now closing.
From graphs to guidance
AI has the potential to change all of this — because at a fundamental level, the function of AI is to automate expertise.
On the health side, that expertise might be the reasoning that lets your internist recognize pneumonia from a stethoscope exam, or the experience that helps a diabetes educator adjust insulin doses, or the pattern recognition that guides a trainer in adjusting a workout plan.
What now?
Generative AI — the newest and most visible form — extends this by communicating that expertise in plain language, personalized to you, and in whatever language you speak. It can translate professional judgment into accessible advice, continuously and at scale.
From expertise to daily coaching
It’s easy to imagine “digital coaches” only as products for athletes and early adopters (and I’ll talk about common consumer coaches in a future post). But that’s no longer true. Increasingly, these systems are performing core healthcare tasks: monitoring vital signs, interpreting results, adjusting treatment, and recommending next steps — functions that were once the exclusive domain of doctors and nurses.
A few examples:
Dexcom Stelo OTC glucose monitor
Dexcom, best known for its continuous glucose monitors, has recently launched a generative AI platform that builds personalized guidance on top of real-time glucose data. Combined with partners like January AI, these systems analyze thousands of data points each day to prompt insulin users on when to eat, dose, or exercise — automating a large part of diabetes management that once required professional oversight.
Teladoc Health, including the formerly-independent Livongo platform for diabetes management, connects glucose meters with AI-driven analysis and messaging. It reviews each reading in real time, recommends behavioral or medication adjustments, and alerts clinicians only when values become dangerous. The daily interpretation and medication titration that once required endocrinology visits now happens automatically, at home, for hundreds of thousands of patients.
Omada Health, which filed for an IPO in 2025, extends that model to hypertension, diabetes prevention, and weight management. Using connected blood-pressure cuffs, scales, and continuous engagement through its app, Omada’s system flags concerning trends and adapts guidance between visits. What used to be a doctor’s or nurse’s job — monitoring, advising, adjusting — has been absorbed by software and remote coaches.
Each of these systems moves core medical interpretation — reading results, identifying patterns, advising action — out of the clinic and into the consumer domain. They aren’t about optimizing athletic performance; they’re about replacing routine clinical decision-making with continuous, automated guidance.
Disruption That Shrinks Healthcare
Christensen described how disruption begins with "non-consumers" — people not currently served by incumbents — and then advances until it competes head-on.
Digital health coaches started with people we don't usually think of as underserved: people between doctor visits, managing conditions on their own, or simply trying to make sense of the data their devices produce.
Those people may see a doctor once a year, or even three or four times a year — but does that really constitute adequate "service," particularly for those with chronic disease? Another way to think of it: if we could have a physician visiting each of these people every day at home, monitoring trends and adjusting guidance in real time, would outcomes improve?
Well, we're about to find out, because these technologies now make that possible — without the physician.
This is why the pattern matters. Digital health coaches aren't improving access to doctors. They're replacing the interpretive and advisory work doctors do. They're moving clinical judgment — the daily monitoring, pattern recognition, and decision-making that used to require years of training — into software that runs continuously, at scale, at near-zero marginal cost.
For healthcare organizations, the strategic question isn't whether to adopt these tools. It's whether the work your clinicians do today will still require a clinician tomorrow — and if not, what you'll do instead.
The most transformative technologies don't make healthcare better.
They make us need it less.
That's not a threat to resist. It's a reality to navigate. The organizations that thrive will be those that recognize which clinical tasks are moving out of their walls, partner with or build the platforms that automate them, and refocus their talent on the complex, high-stakes work that still requires human judgment.
The question for every healthcare executive reading this: what are you doing today that software will do tomorrow — and what will your organization do that software can't?
Note: in a future post, I’ll explore how consumer-focused digital coaches are reshaping wellness for everyone—not just patients.